Menu
Menu

Children with concerns are initially seen with family in a scheduled consultation with the Neurodevelopmental Pediatrician at Pratheeksha Out Patient department. Prior appointments are taken from Pratheeksha reception. Consultation deals with history taking and examination. Family will be then guided for assessments. Results and possible diagnosis will be discussed with the family in the review visit and a treatment plan will be derived in consensus with them.
Professor and Incharge of CDC (MBBS, DNB Pediatrics, PGD Development Neurology, Fellowship in Neurology (Pune), Fellowship in Epileptology (Japan). She has over 16 years of experience in the field of Child Development Neurology and Epilepsy. Recipient of many vocational Excellence Awards, Writer and Motivational Speaker and lead founder of Pratheeksha CDC.
Assistant Professor (MBBS, MD Pediatrics, Fellow Neuro Developmental Behavioral Pediatrics fNDBP (IAP). She joined Pratheeksha in 2021. She has around 8 years of experience in General pediatrics - Outpatient and critical care management of sick children and now her focus is on Developmental and Behavioral Pediatrics. She secured second rank in the All India Fellowship exit examination in NDBP. She has an empathetic and professional attitude committed to optimum patient care.
Consultations available on MONDAYS, TUESDAYS,THURSDAYS & SATURDAYS (9am -2pm) with Prior appointments. Afternoon Op Consultation on all Wednesdays from 3 pm to 6 pm.

The child will be directed for age-appropriate assessments based on their concerns. Assessments are made from parent opinion and observation.
The following are some of them:
Developmental assessment, Speech assessment, Autism screening, Autism diagnostic panel, Physical assessment, Academic skill assessment, IQ, ADHD Panel, Social age assessment, and School readiness assessment (Nursery evaluation scale Trivandrum).
Assessments may have to be rescheduled if the child is too tired/ sleepy/ cranky, to avoid errors in conclusions.

The child may
be subjected to certain basic lab workups related to the brain (eg: haemoglobin,
thyroid status, etc). In addition to
this panel of tests like metabolic workup (TMS, GCMS), EEG, and MRI Brain may be
done for definitive diagnosis. Genetic workup includes Karyotyping, Whole exome
sequencing, Clinical Exome, and Chromosomal Microarray may be done for diagnostic
and Prognostic purposes.
EEG is
preferred in children with a history of seizures, developmental delay, and older
children with ASD, ADHD, and Rett syndrome. In-house EEG is available.
Otoacousticemission (OAE) is routinely done as a screening test for hearing. Brainstem-evoked auditory response (BERA/ ABR) is done to confirm any hearing impairment

Neuroimaging is done to study the structural abnormalities in the brain in a child with developmental delay (especially when there is a history of perinatal asphyxia/eventful birth history), unprovoked seizures, abnormal head sizes, and older children with ASD.
DT is done
by well-experienced developmental therapists in infants and young children with
developmental delays. NDT is a hands-on
technique used to correct and teach movements in children who lack movement.
The target of NDT is to repeatedly expose the child to movements so that the
child can gain movement control and learn to use a wide range of movements.
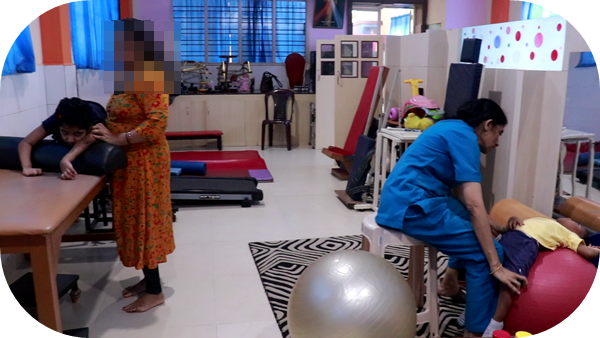
Paediatric physiotherapy treatment is based on many hands-on techniques, exercises and interventions with the goal of addressing functional impairments including muscle tone, strength, coordination, balance and posture, mobility and achieving an optimal range of motion. Treatment is always performed with the ICF model in mind so that activity limitations and participation are addressed. It focuses on treating movement and movement-based disorders (focussing on balance, coordination, posture), gait disorders, and motor developmental delay muscle disorders in children up to 18 years of age. Some techniques include NDT (NeuroDevelopmental Therapy), CIMT (Constraint Induced Movement Therapy) etc focusing on achieving gross motor milestones, managing spasticity, and improving balance and coordination.
We have a handful of success stories of children with cerebral palsy, Downs syndrome, Developmental epileptic encephalopathy, Infantile strokes, spinomuscularatrophy, congenital torticollis, erbs palsy, myopathies/ muscular dystrophies etc who improved in their functional movement abilities.
Several orthoses(like ankle foot orthosis, high ankle foot knee orthosis, and foot arch supports), function-improving aids (corner seats), high chairs and ambulatory aids like walkers, and wheelchairs are customised and used appropriately.
Botox injections, antispastic medications, Vojta technique, and functional electrical stimulations are done in indicated children. The availability of Physical Medicine and rehabilitation specialists adds to the benefits of these children.

Pediatric speech-language pathologists work to help children communicate effectively by assisting with the improvement of their verbal and non-verbal language skills. They also help with things like feeding and swallowing abilities. They focus on improving three areas of communication: Speech (children’s articulation, decrease stuttering/dysfluency, or treat voice disorders), Receptive (helping children process and understand the information they’re receiving from others) and expressive Language (how to produce words and combine words into phrases and sentences to outwardly communicate their wants and needs and share information).

Occupational therapists work with children in the following areas:

Special
education focuses on students with developmental disabilities, ranging from
mild to moderate. They include learning disability, ADHD, Attention deficit
disorders, and Intellectual disability. Remedial education supports the child in
accessing the mainstream education and curriculum, and not exactly the classroom
content. We conduct individual and group sessions (GET SMART JUNIOR, SENIOR)
along with intensive vacation camps for children with learning disability/
difficulties. Sessions are decided after doctor consultation and detailed
assessments. Sessions are available from Monday to Saturday (9 am -5 pm).
Appropriate school formalities like Attendance allowance during school hours
and LD certifications will be issued accordingly.

AET focuses on tasks
and activities which help enhance learning,
communication ability, attention, memory, and academic performance in children. These are individual sessions. Conventionally AET
includes brain gym movement-based and sheet activities. Certain children may
require stimulant medications under the supervision of a neurodevelopmental
paediatrician.

Recently Pratheeksha launched a
Virtual Reality technology that can be used to remove distractions and
provide environments that get the subjects' attention and increase their
ability to concentrate. Virtual Reality technology can hold a patient's
attention for a longer period of time than other methods can because VR is
immersive, interactive and imaginal.

Multi-sensory
therapy is an activity which usually takes place in a dedicated room where
patients experience a range of patterned visual, auditory, olfactory and
tactile stimuli . The room has coloured spotlights, a projector, fibre-optic
sprays or curtains, bubble tubes, a music system, an aromatherapy diffuser,
panels of interactive knobs and switches that trigger sounds or lights when
activated; and a variety of hand-held objects that offer particular tactile or
visual sensations to the patient. MST is particularly useful in children with
Autism spectrum disorder, sensory processing disorder, and ADHD. Optical,
acoustic, olfactory and tactile stimuli help hyperactive individuals learn how
to direct their focus, and how to deal with real-life encounters in a healthy
way. Children with tactile and auditory sensitivities, toe walking, and gravitational insecurities benefit from MST.

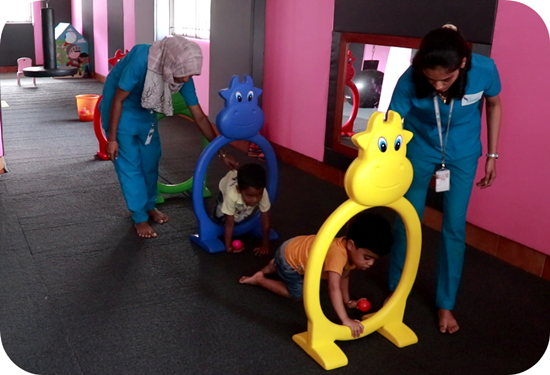
Play therapy allows
children to communicate their experiences and feelings through play. It is a one-on-one session with the parent and child where the parents are trained to
associate and interact with a child through play.
Parents are
the full-time ‘therapists’ available for the child. Hence PMT focuses on
improving parenting skills for optimum benefits for the child. PMT are
conducted in various sessions like ADL skill training (toilet training, sleep
routine), tantrum management, management of sensory problems etc. When parents become trained in behaviour therapy, they learn
skills and strategies to help their child with ADHD succeed at school, at home,
and in relationships.